Introduction
Leg ulcers are a common and often painful condition that can significantly impact an individual’s quality of life. In particular, leg ulcers early stages are crucial to identify, as timely intervention can prevent further complications and promote faster healing. These ulcers, commonly referred to as venous ulcers, primarily affect the lower legs and are a result of poor blood circulation. In this article, we will explore the signs and symptoms of leg ulcers in the early stages, discuss possible causes, and provide insights into effective treatments to manage this condition.
What are Leg Ulcers?
Leg ulcers are open sores or wounds that occur on the skin of the lower legs. These ulcers can develop for various reasons, but the most common type is venous ulcers, which result from poor circulation in the veins of the legs. When the blood flow is obstructed or inadequate, the skin becomes more prone to injury and can eventually form an ulcer. The early stages of leg ulcers are often characterized by subtle symptoms that may go unnoticed if not properly addressed.
Recognizing the Early Stages of Leg Ulcers
The initial stages of leg ulcers are not always obvious. The symptoms often develop gradually, and patients may dismiss them as minor irritations or conditions that will heal on their own. However, it’s essential to be aware of the early warning signs to prevent the ulcers from worsening. Here are some key indicators of leg ulcers in their early stages:
- Swelling and Heaviness: Swelling in the legs is one of the first signs of venous insufficiency. The legs may feel heavy or fatigued, especially after standing or walking for long periods.
- Skin Discoloration: The skin around the ankle may become discolored, ranging from red to brownish hues. This change occurs due to poor circulation and the buildup of blood in the veins.
- Itching and Dry Skin: As the blood flow decreases, the skin may become dry, flaky, and irritated. This can lead to itching, which may worsen as the condition progresses.
- Pain and Tenderness: In the early stages, you may notice a dull ache or throbbing pain in the affected area. This pain may be more pronounced when standing or walking.
- Appearance of Small Blisters: Small blisters or open sores may start to appear on the skin. These blisters can rupture and become larger wounds if left untreated.
Causes of Leg Ulcers
Venous ulcers are primarily caused by poor circulation in the veins. Several factors can contribute to this, including:
- Chronic Venous Insufficiency (CVI): CVI occurs when the veins in the legs are unable to efficiently return blood to the heart. This leads to increased pressure in the veins, which can damage the surrounding tissue and result in an ulcer.
- Varicose Veins: Enlarged and twisted veins in the legs can impede blood flow and increase the risk of developing leg ulcers.
- Blood Clots: A history of blood clots or deep vein thrombosis (DVT) can damage the veins and lead to venous ulcers.
- Obesity: Excess weight puts additional strain on the veins, making it harder for blood to flow properly.
- Diabetes: People with diabetes are more prone to developing ulcers due to poor circulation and slower healing.
- Age: Older adults are more susceptible to leg ulcers, as their skin becomes thinner and less elastic with age, making it easier for ulcers to form.
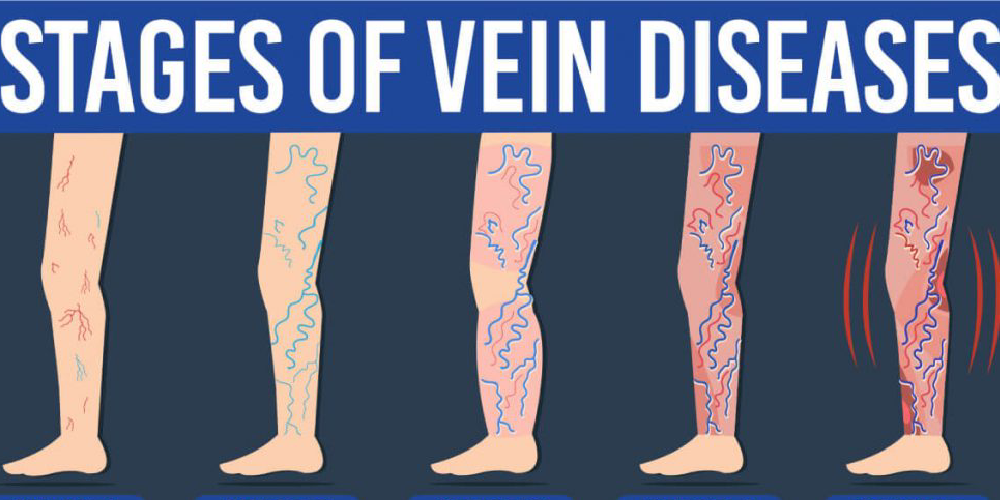
The Progression of Leg Ulcers
If left untreated, leg ulcers early stages can progress into more severe ulcers that are difficult to heal. Here’s a look at the different stages of venous ulcers:
- Stage 1: Early Symptoms: As mentioned earlier, swelling, skin discoloration, and itching are early signs of venous insufficiency. At this stage, the skin may still appear intact, but the underlying circulation problems are beginning to take hold.
- Stage 2: Formation of Open Sores: As the condition progresses, small sores or blisters may appear on the skin. These sores may be painful and tender to the touch. The surrounding skin may also appear red and inflamed.
- Stage 3: Large, Deep Ulcers: In the later stages, the sores become larger and deeper, with visible tissue damage. The skin may be necrotic (dead), and the ulcer can produce a significant amount of discharge.
- Stage 4: Chronic Ulcers: If left untreated, leg ulcers can become chronic, meaning they may take months or even years to heal. At this stage, the ulcers may require advanced treatments like surgery or long-term wound care.
Treatment Options for Leg Ulcers
The key to treating leg ulcers is addressing the underlying circulation problems while also promoting wound healing. Early intervention is critical for preventing the ulcers from becoming larger and more difficult to treat. Here are some common treatment options:
1. Compression Therapy
Compression therapy involves using specially designed bandages or stockings to apply gentle pressure to the affected leg. This helps improve blood flow and reduces swelling. Compression therapy is often the first-line treatment for venous ulcers and is most effective when started in the early stages.
2. Wound Care and Dressings
Proper wound care is essential for promoting healing and preventing infection. The ulcer should be cleaned regularly, and appropriate dressings should be applied to protect the wound and encourage tissue regeneration. Advanced dressings such as hydrocolloid or foam dressings may be used for optimal results.
3. Medications
In some cases, medications may be prescribed to manage symptoms such as pain or inflammation. Topical antibiotics may be used to prevent infection, while pain relievers can help manage discomfort.
4. Surgical Intervention
In severe cases, surgery may be required to address the underlying venous insufficiency. This could involve procedures like vein stripping or the removal of varicose veins. In rare cases, skin grafts may be necessary to promote healing.
5. Lifestyle Changes
Maintaining a healthy lifestyle can play a significant role in preventing and managing leg ulcers. Regular exercise, weight management, and avoiding prolonged standing or sitting can all help improve circulation and reduce the risk of developing ulcers.
How to Prevent Leg Ulcers
Preventing leg ulcers involves taking proactive steps to manage circulation and maintain healthy skin. Here are a few strategies to reduce your risk:
- Practice good skincare: Keep your skin moisturized and clean to prevent irritation.
- Elevate your legs: Elevate your legs whenever possible to reduce swelling and improve blood flow.
- Wear compression stockings: These help support healthy circulation and prevent fluid buildup.
- Exercise regularly: Activities like walking and swimming can promote blood circulation in the legs.
Conclusion
Recognizing leg ulcers early stages is crucial for preventing the progression of the condition and minimizing complications. If you notice symptoms such as swelling, skin discoloration, or pain in your legs, it’s essential to seek medical advice promptly. With the right treatment, many leg ulcers can heal effectively, and the risk of future ulcers can be minimized. Taking proactive steps to manage circulation, maintain a healthy lifestyle, and seek professional care will help ensure better outcomes for individuals affected by venous ulcers.