What are CAR T Cells?
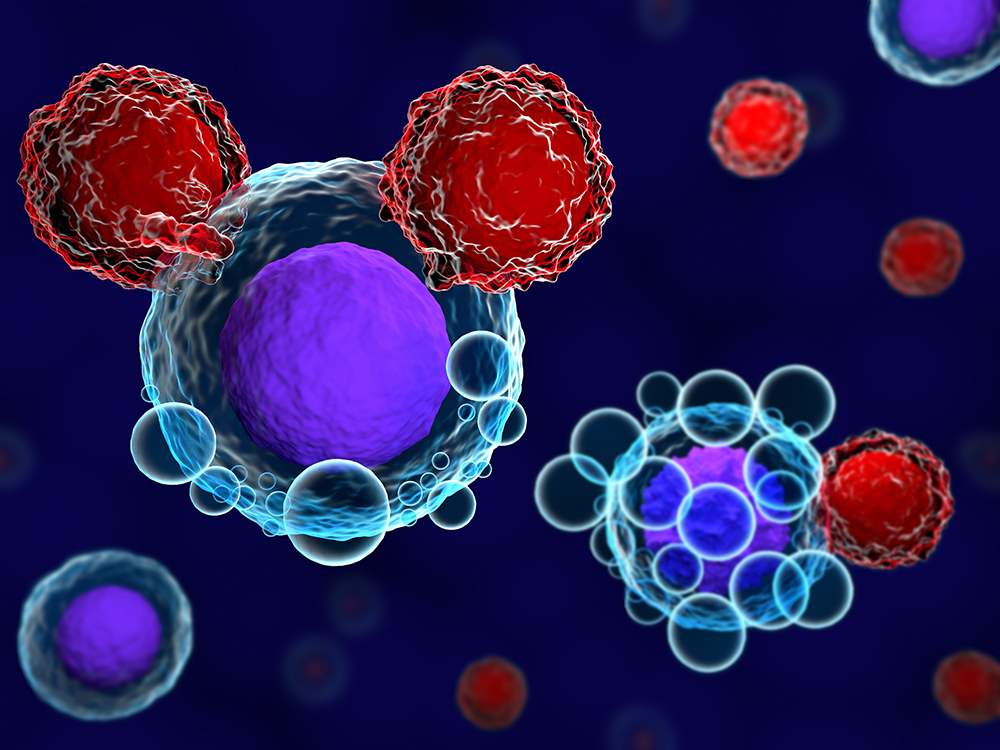
Chimeric antigen receptor (CAR) T cell therapy is a type of immunotherapy that uses modified T cells to attack cancer cells. In this therapy, a patient’s own T cells are collected and genetically engineered to express a chimeric antigen receptor (CAR) on their surface. This CAR bonds to a specific protein (antigen) on the surface of a patient’s tumor cells. When reinfused into the patient, the CAR T cells can then identify and attack the cancer cells that express that specific antigen on their surface.
How CAR T Cells are Produced?
To produce CAR T cells, T cells are first collected from a patient’s blood through a process called leukapheresis. The collected T cells are then sent to a manufacturing facility where they are genetically engineered using a virus to insert the gene for the CAR into the T cells. The CAR includes an extracellular antigen binding domain, usually derived from an antibody that binds to a specific antigen on the tumor cell. It is connected to intracellular T cell activation domains that trigger the immune properties of the modified T cells. The engineered CAR T cells are then multiplied into billions of copies through a process called expansion before being infused back into the patient’s bloodstream.
Targets of CAR T Cell Therapy
They has been approved for treating several types of blood cancers that express specific antigens on their cell surface including:
– Acute Lymphoblastic Leukemia (ALL): CAR T cells are engineered to target the CD19 antigen which is expressed on B cells including ALL cells.
– Lymphoma: Both Non-Hodgkin’s and Hodgkin’s lymphomas can be targeted with CD19 CAR T cells since they originate from B cells which express CD19.
– Multiple Myeloma: This cancer of plasma cells can be targeted using CAR T cells engineered to bind to B-cell maturation antigen (BCMA) which is highly expressed on myeloma cells.
– Other Potential Targets: Research is ongoing to develop it against other antigen targets expressed in blood cancers like CD20, CD22, and CD30 as well as solid tumors like mesothelin, HER2, and others.
How CAR T Cell Therapy Works
Once infused back into the patient, the CAR T cells start circulating throughout the body and are able to identify and bind to their antigen target on cancer cells. This triggers the activation of the CAR T cells which leads to:
– Proliferation and Expansion: The activated CAR T cells rapidly proliferate and expand in vivo forming large clusters that attack the tumor.
– Cytokine Release: Activated CAR T cells secrete pro-inflammatory cytokines like interferon-γ and interleukin-2 at the tumor site which further triggers and attracts an immune response.
– Killing of Cancer Cells: The activated CAR T cells employ two main mechanisms to kill antigen-expressing tumor cells – release of cytotoxic granules containing perforin and granzymes, and expression of Fas ligand (FasL) which triggers the Fas death receptor apoptotic pathway in cancer cells.
– Long-Term Persistence: Some CAR T cells survive for months or years as memory cells keeping the patient in long-term remission by continued surveillance for antigen-expressing cancer cells.
Clinical Effectiveness of CAR T Cell Therapy
Clinical trials have shown they can produce high complete response rates against hematological cancers. Some key results include:
– FDA-approved anti-CD19 CAR T Cell Therapies tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) have response rates over 50% in relapsed/refractory ALL and diffuse large B cell lymphoma (DLBCL).
– In multiple myeloma, a 93% response rate was seen with anti-BCMA CAR T therapy idecabtagene vicleucel in a trial of heavily pretreated patients.
– Durable responses lasting several years have been observed in some patients suggesting CAR T cells can provide a potential cure for some blood cancers.
– CAR T therapy is also being studied in combination with other immunotherapies and chemotherapy to increase responses rates further.
Potential Challenges and Side Effects
While revolutionary in cancer treatment, CAR T cell therapy does have some challenges and potential side effects that require careful management:
– Cytokine Release Syndrome: High levels of inflammatory cytokines released by activated CAR T cells can sometimes lead to fever, nausea, low blood pressure and other symptoms of CRS which are usually temporary but rarely life-threatening.
– Neurotoxicity: In some patients, cytokines released during CRS can cause neurologic symptoms ranging from headaches to confusion and seizures due to brain swelling, though again usually temporary.
– Limited Persistence: While some CAR T cells persist long-term, others may disappear within months requiring repeat or salvage therapy for relapsed/refractory disease.
– Manufacturing Challenges: Large scale manufacturing of CAR T cell products is complex and expensive requiring specialized facilities and expertise.
– Limited to Target Antigens: Success of CAR T cell therapy depends on the cancer uniformly expressing the target antigen, but target loss occurs sometimes leading to relapse.
– Side Effects of Long-term B Cell Aplasia: Some lasting side effects can occur from long-term B cell depletion after CD19 CAR T therapy like increased risk of infections.
Get More Insights on CAR T Cell Therapy
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc.